ILC Program of Excellence “Clinical ILC Team”
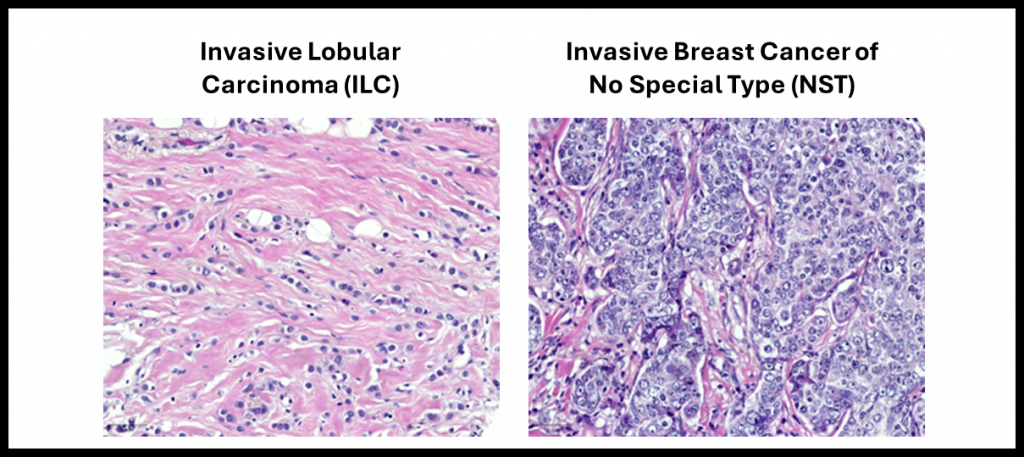
The histologic growth pattern of invasive lobular breast cancer (ILC) shows a hallmark single file pattern compared to the more cohesive growth pattern seen in invasive ductal breast cancer, or breast cancer of no special type (NST). This is due to the loss of the membranous cell adhesion protein E-cadherin in ~90% of all ILCs, and leads to more difficult diagnosis on imaging.
UPMC has a large multidisciplinary clinical program for the treatment of all breast cancer stages and types (https://www.upmc.com/services/breast). We are fortunate to have several clinicians focusing on ILC. Further, the L-O Lab has a number of exciting collaborative studies with physician-scientists at UPMC/Pitt.
Medical Oncology
Dr. Julia Foldi

Julia Foldi, MD, PhD, is an Assistant Professor of Medicine in the Division of Malignant Hematology and Medical Oncology at the University of Pittsburgh School of Medicine and the UPMC Hillman Cancer Center and a Breast Medical Oncologist at the Magee Womens Cancer Center. She treats patients with all types and stages of breast cancer, but is particularly focused on ILC. She works closely with basic science and translational investigators to design prospective clinical trials and correlative studies to address the unmet needs of patients with ILC.
Some of Dr. Foldi’s specific research projects dedicated to ILC include:
- Identifying increased late recurrence in ILC in four large National Surgical Adjuvant Breast and Bowel Project (NSABP) randomized clinical trials,
- Foldi J et al. Long-term outcomes by lobular versus ductal histology in four NSABP adjuvant breast cancer trials. J Natl Cancer Inst. 2024 Aug 10:djae188. PMID: 39128018.
- Development of a molecular RNA suquencing-based signature of late distant recurrences in patients with early-stage ILC (ongoing)
- Investigating the role of liquid biopsies and circulating tumor DNA testing in patients with ILC, both metastatic and early-stage
- Foldi J et al. Personalized circulating tumor DNA testing for detection of progression and treatment response monitoring in patients with metastatic invasive lobular carcinoma of the breast. JCO Precis Oncol 9, e2400577(2025). DOI:10.1200/PO-24-00577 PMID: 40324116
- Foldi J et al. Serial circulating tumor DNA (ctDNA) monitoring in early-stage, HR+/HER2-, invasive lobular carcinoma (ILC) of the breast and impact on clinical outcomes. JCO 43, 581-581(2025). DOI:10.1200/JCO.2025.43.16_suppl.581
- LBC-Monitor Clinical Trial (HCC 24-096; NCT06666439) – Liquid Biopsy to Monitor Treatment Response for Women with Metastatic Lobular ER+ Breast Cancer.
- Evaluating the utility of a personalized circulating tumor DNA assay in monitoring treatment response in women starting first line endocrine-based treatment for newly diagnosed metastatic lobular breast cancer. This study is currently recruiting at UPMC Magee-Womens Hospital.
Here is a link to Dr. Foldi’s ILC publications
Dr. Marija Balic

UPMC breast medical oncologist Marija Balic, MD, PhD, MBA is actively engaged in both the clinical and research components of breast cancer. Dr. Balic is chief of Medical Breast Oncology at Magee-Womens Cancer Center and the co-director of UPMC Comprehensive Breast Center. She is also professor in the Department of Medicine, Division of Hematology/Oncology at the University of Pittsburgh and Scientific Director of the NSABP Foundation Translational Research Program. She has a longstanding interest in ILC and the role of liquid biopsy to improve its detection and molecular characterization.
Some of Dr. Balic’s papers investigating ILC include:
- Better understanding the molecular landscape of metastatic lobular breast cancer and the impact of transcriptomic subtypes in primary ER+ ILC on immune infiltration.
- Dandachi N et al. Deciphering the molecular landscape of metastatic lobular breast cancer. EBioMedicine. 2022 Dec;86:104385. doi: 10.1016/j.ebiom.2022.104385. Epub 2022 Nov 28. PMID: 36455408; PMCID: PMC9706609.
- Chen F, et al. Immune infiltration correlates with transcriptomic subtypes in primary estrogen receptor positive invasive lobular breast cancer. NPJ Precis Oncol. 2024 Nov 9;8(1):257. doi: 10.1038/s41698-024-00746-z. PMID: 39521942; PMCID: PMC11550424.
- Investigating long-term clinical outcomes in patients with invasive lobular breast cancers treated on four large National Surgical Adjuvant Breast and Bowel Project (NSABP) randomized clinical trials
- Foldi J, et al. Long-term outcomes by lobular versus ductal histology in four NSABP adjuvant breast cancer trials. J Natl Cancer Inst. 2024 Aug 10:djae188. PMID: 39128018.
Here is a link to Dr. Balic’s ILC publications.
Breast Surgical Oncology
Dr. Priscilla McAuliffe

Priscilla McAuliffe, MD, PhD, FACS, FSSO is a breast surgical oncologist at UPMC Hillman Cancer Center and an associate professor of surgery at the University of Pittsburgh School of Medicine. She treats patients with all breast diseases, with a special interest and research emphasis on ILC, pre-invasive neoplasms including LCIS, premenopausal and older patients with breast cancer, breast conservation therapy and locally advanced breast cancer.
Dr. McAuliffe together with Dr. Rachel Jankowitz, Director of the Rena Rowan Breast Center and a medical oncologist at Penn Medicine, completed the first ever clinical trial exclusively for patients with ILC. This study aimed to learn more about how three commonly prescribed anti-estrogen therapies affect the tumor tissue of patients diagnosed with ILC (clinical trial info here)
Additionally, Dr. McAuliffe has a particular interest in “right-sizing” surgical care for patients with ILC and other breast cancer – specifically in older patients. In general, patients with ILC are diagnosed at later ages than those with invasive ductal cancer, making these questions particularly salient. She has evaluated the applicability of the Choosing Wisely guidelines (omission of axillary surgery for certain patients aged 70 years old and older) for patients with ILC, and she has recently completed a prospective trial demonstrating a decrease in low-value care for older patients.
Lastly, Dr. McAuliffe has created close collaborations with both ILC survivors/advocates, and with basic science researchers. She created and leads a program in which excess tumor tissue and blood, generously donated by patients, can be quickly delivered from the operating room to the laboratory for study. This program has resulted in the establishment of patient-derived organoids, specifically from patients with ILC, allowing direct analysis of the surgical tissues themselves. Her role also includes educating the next generation of physician scientists.
Some of Dr. McAuliffe’s interests and recent publications on ILC include:
- Clinical characterization of ILC subtypes, including upgrade rates of variant LCIS compared to classic LCIS diagnosed in core needle biopsies, and the similarity of mixed invasive ductal lobular carcinoma to ILC compared to NST.
- Harinath L et al. Upgrade Rates of Variant Lobular Carcinoma In Situ Compared to Classic Lobular Carcinoma In Situ Diagnosed in Core Needle Biopsies: A 10-Year Single Institution Retrospective Study. Mod Pathol. 2024 Apr;37(4):100462. doi: 10.1016/j.modpat.2024.100462. Epub 2024 Feb 28. PMID: 38428736.
- Nasrazadani A et al. Mixed invasive ductal lobular carcinoma is clinically and pathologically more similar to invasive lobular than ductal carcinoma. Br J Cancer. 2023 Apr;128(6):1030-1039. doi: 10.1038/s41416-022-02131-8. Epub 2023 Jan 5. PMID: 36604587; PMCID: PMC10006180.
- Transcriptomic and spatial molecular profiling in invasive lobular carcinoma.
- Puthanmadhom S et al. Transcriptomic analysis identifies enrichment of cAMP/PKA/CREB signaling in invasive lobular breast cancer. Breast Cancer Res. 2024 Oct 30;26(1):149. doi: 10.1186/s13058-024-01900-y. PMID: 39478577; PMCID: PMC11526681.
- Shah OS, et al. Spatial molecular profiling of mixed invasive ductal and lobular breast cancers reveals heterogeneity in intrinsic molecular subtypes, oncogenic signatures, and mutations. Proc Natl Acad Sci U S A. 2024 Jul 30;121(31):e2322068121. doi: 10.1073/pnas.2322068121. Epub 2024 Jul 23. PMID: 39042692; PMCID: PMC11295029.
- De-intensification of axillary surgery in patients with ILC.
- Carleton N, et al. Is the Choosing Wisely Recommendation for Omission of Sentinel Lymph Node Biopsy Applicable for Invasive Lobular Carcinoma? Ann Surg Oncol. 2022 Sep;29(9):5379-5382. doi: 10.1245/s10434-022-12003-3. Epub 2022 Jun 13. PMID: 35697956; PMCID: PMC10257800.
- Carleton N, et al. Electronic Health Record-Based Nudge Intervention and Axillary Surgery in Older Women With Breast Cancer: A Nonrandomized Controlled Trial. JAMA Surg. 2024 Oct 1;159(10):1117-1125. doi: 10.1001/jamasurg.2024.2407. PMID: 39018053; PMCID: PMC11255976.
Here is a link to Dr. McAuliffe’s ILC publications.
Breast Pathology
Dr. Rohit Bhargava

Rohit Bhargava, MBBS is the Chief of Pathology at UPMC Magee-Womens Hospital and Professor of Pathology at the University of Pittsburgh School of Medicine. Dr. Bhargava is an experienced breast pathologist and specializes in diagnostic histopathology and immunohistochemistry. He is actively involved in identifying novel diagnostic and prognostic markers for breast cancer, predictive biomarkers in breast carcinoma and their correlation to clinical outcomes and has specific interest in studying invasive lobular breast cancer. His involvement with projects in the Lee-Oesterreich Lab has been critical in bringing the clinical focus of ILC projects to the forefront.
Some of Dr. Bhargava’s papers investigating ILC include:
- Spatial molecular profiling of mixed invasive ductal-lobular breast cancers, and clinicopathologic and genomic features of lobular like invasive mammary carcinoma.
- Shah OS, et al. Spatial molecular profiling of mixed invasive ductal and lobular breast cancers reveals heterogeneity in intrinsic molecular subtypes, oncogenic signatures, and mutations. Proc Natl Acad Sci U S A. 2024 Jul 30;121(31):e2322068121. doi: 10.1073/pnas.2322068121. Epub 2024 Jul 23. PMID: 39042692; PMCID: PMC11295029.
- Yu J, et al. Clinicopathologic and genomic features of lobular like invasive mammary carcinoma: is it a distinct entity? NPJ Breast Cancer. 2023 Jul 13;9(1):60. doi: 10.1038/s41523-023-00566-7. PMID: 37443169; PMCID: PMC10345141.
- Upgrade rates of variant LCIS compared to classic LCIS diagnosed in core needle biopsies.
- Harinath L, et al. Upgrade Rates of Variant Lobular Carcinoma In Situ Compared to Classic Lobular Carcinoma In Situ Diagnosed in Core Needle Biopsies: A 10-Year Single Institution Retrospective Study. Mod Pathol. 2024 Apr;37(4):100462. doi: 10.1016/j.modpat.2024.100462. Epub 2024 Feb 28. PMID: 38428736.
- The importance of standardization of histopathologic diagnosis of ILC based on a worldwide study of histopathologic diagnostic criteria.
- De Schepper M, et al. Results of a worldwide survey on the currently used histopathological diagnostic criteria for invasive lobular breast cancer. Mod Pathol. 2022 Dec;35(12):1812-1820. doi: 10.1038/s41379-022-01135-2. Epub 2022 Aug 3. PMID: 35922548; PMCID: PMC9708574.
- The clinical and diagnostic features of ILC.
- Nasrazadani A, et al. Mixed invasive ductal lobular carcinoma is clinically and pathologically more similar to invasive lobular than ductal carcinoma. Br J Cancer. 2023;128:1030-1039. PMID: 36604587.
- Jing Yu, et al. Classical Type Invasive Lobular Carcinoma with HER2 Overexpression: Clinical, Histological and Hormone Receptor Characteristics. Am J Clin Pathol. 2011 Jul;136(1):88-97. PMID: 21685036.
- Jing Yu, et al. Invasive lobular carcinoma with extracellular mucin production and HER-2 overexpression: a case report and further case studies. Diagnostic Pathology. 2010;5:36. PMID: 20550696.
- Dabbs, et al. Lobular versus ductal breast neoplasms: The diagnostic utility of p120 catenin in the breast and in metastatic tumors. Am J Surg Pathol. 2007 Mar;31(3):427-437. PMID: 17325485.
Here is a link to Dr. Bhargava’s ILC publications.
Screening
Wendie A. Berg, MD, PhD

1) General advances in screening
Wendie A. Berg, MD, PhD’s work defines where supplemental imaging adds meaningful cancer yield beyond mammography, and what trade-offs to expect. In the clinical trial ACRIN 6666, adding annual screening ultrasound to mammography in women at elevated risk increased detection of mostly small, node-negative invasive cancers; a single screening MRI found still more cancers missed by both tests (with higher recalls/biopsies), establishing a risk-adapted, multimodal paradigm.
She has also led prospective evaluation of contrast-enhanced mammography (CEM) as an alternative to MRI. In the multicenter SCEMAM trial, CEM alone identified additional invasive cancers (several lobular) that other modalities missed, supporting CEM as a practical, high-sensitivity option in dense-breast and personal-history cohorts.
Complementing these anatomic/contrast studies, Dr. Berg’s positron-based work showed high accuracy of positron emission mammography (PEM) for primary breast cancer and characterized histology-specific FDG uptake, lower in ILC/DCIS than in high-grade IDC, which helps explain performance differences of functional imaging across subtypes.
- Berg WA, et al. Detection of breast cancer with addition of annual screening ultrasound or a single screening MRI to mammography in women with elevated breast cancer risk. JAMA. 2012;307(13):1394-1404 PMID: 22474203 PMCID: PMC3891886 DOI: 10.1001/jama.2012.388
- Berg WA, et al. Screening for Breast Cancer with Contrast-enhanced Mammography as an Alternative to MRI: SCEMAM Trial Results. Radiology. 2025;315(3):e242634. PMID: 40525975 DOI: 10.1148/radiol.242634
- Berg WA, et al. High-resolution FDG PET with compression (“positron emission mammography”) is highly accurate in depicting primary breast cancer. Breast J. 2006;12(4):309-323. doi: 10.1111/j.1075-122X.2006.00269.x.PMID: 16848840
- Kalinyak JE, et al. Breast cancer detection using high-resolution breast PET compared to whole-body PET or PET/CT. Eur J Nucl Med Mol Imaging. 2014;41(2):260-275. PMID: 24085500 DOI: 10.1007/s00259-013-2553-1
2) Focus on invasive lobular carcinoma (ILC) & lobular neoplasia
Dr. Berg has repeatedly documented mammography’s reduced sensitivity for ILC, which contributes to later or larger presentations; in preoperative staging, mammography detected 34% of ILC vs 81% of IDC, reinforcing the need for adjunct imaging pathways.
Evidence from ACRIN 6666 and subsequent practice-pattern data underscores that ultrasound, MRI, and CEM can help close ILC’s detection gap; a recent survey of breast radiologists reports broad support for imaging beyond mammography when screening or staging ILC.
For lobular neoplasia, Dr. Berg has co-authored management studies showing higher upgrade risk for LCIS (especially variant LCIS, pleomorphic/florid) than for atypical lobular hyperplasia, supporting selective surgical excision; her guidance on image-guided biopsy also outlines when excision is generally warranted for high-risk lesions.
- Berg WA, Gutierrez L, NessAiver MS, et al. Diagnostic accuracy of mammography, clinical exam, ultrasound, and MRI in preoperative assessment of breast cancer. Radiology. 2004;233(3):830-849. PMID: 15486214 DOI: 10.1148/radiol.2333031484
- Coffey K, Berg WA, Dodelzon K, et al. Breast Radiologists’ Perceptions on the Detection and Management of Invasive Lobular Carcinoma: Most Agree Imaging Beyond Mammography Is Warranted. J Breast Imaging. 2024;6(2):157-165. PMID: 38340343 PMCID: PMC10983784 DOI: 10.1093/jbi/wbad112
- Sen LQ, Berg WA, Hooley RJ, et al. Core Breast Biopsies Showing Lobular Carcinoma In Situ Should Be Excised and Surveillance Is Reasonable for Atypical Lobular Hyperplasia. AJR Am J Roentgenol. 2016;207(5):1132-1145. PMID: 27532153 DOI: 10.2214/AJR.15.15425
- Harinath L, Villatoro TM, Clark BZ, et al. (incl. Berg WA). Upgrade Rates of Variant Lobular Carcinoma In Situ Compared to Classic LCIS Diagnosed in Core Needle Biopsies: A 10-Year Single-Institution Retrospective Study. Mod Pathol. 2024;37(4):100462. PMID: 38428736 DOI: 10.1016/j.modpat.2024.100462