Our Story in ILC Research Excellence
When moving from Baylor College of Medicine, Houston, TX, to UPCI/Magee Womens Research Institute, Dr. Oesterreich had just become interested in ILC, as some estrogen receptor cofactors were expressed higher in ER+ ILC (as per Oncomine). She decided to start researching ILC, and was delighted to learn that Dr. David Dabbs, the Chief Pathologist at UPMC Magee-Womens Hospital was an internationally recognized expert in ILC. The ILC studies would not have been possible without Dr. Dabbs advice and countless slide reviews. Dr. Oesterreich and Dr. Dabbs had many productive collaborations, and also co-authored a review in “Breast Pathology, 2nd Edition by David J. Dabbs”.
After some unsuccessful attempts to obtain NIH funding, Dr. Oesterreich received BCRF funding for her ILC research. This allowed the journey to start. We increased research on ILC, with the support of some exceptional students, postdocs and Dr. Nancy Davidson, at the time Dr. Oesterreich’s main mentor. Of note BCRF also provided funds for subsequent ILC Symposia, and started to include ILC into Breakout sessions at the Annual BCRF Symposium.
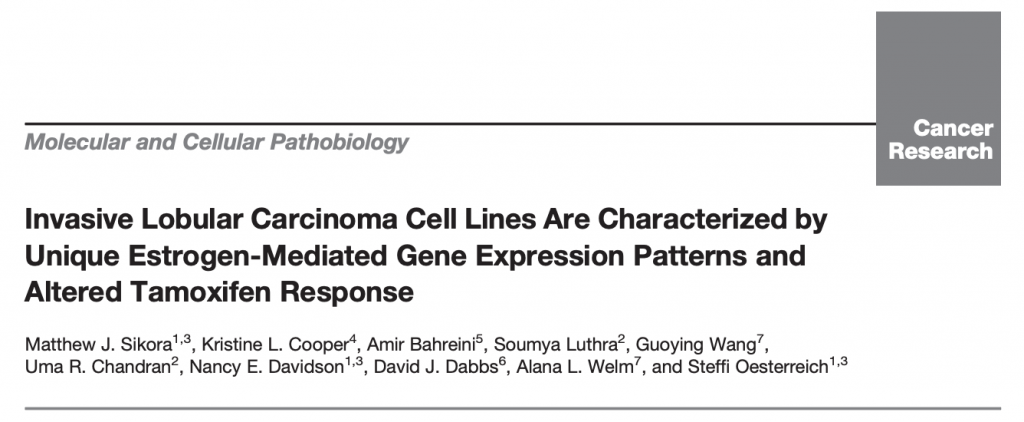
This foundational study established that invasive lobular carcinoma (ILC) cell lines exhibit unique estrogen-mediated transcriptional programs and distinct tamoxifen responses compared to ductal models. Led by Dr. Matthew Sikora during his postdoctoral training in the Oesterreich–Lee laboratory, the work included collaborations with multiple Pitt faculty and collaborators such as Dr. Alana Welm (Utah), providing the first systematic evidence for differential estrogen signaling in ILC. Dr. Sikora is now Associate Professor at UC and is continuing work on ILC.
After many discussions and guidance from Dr. Davidson, we opened the first clinical trial specifically in ILC: a biomarker window trial aimed at improving understanding of endocrine therapy in patients with ILC. It was performed with the help of the Translational Breast Cancer Research Consortium (TBCRC). Drs. Rachel Jankowitz and Priscilla McAuliffe are clinical PIs. Dr. Jankowitz received a Career Development Award from Susan G. Komen supporting the study.
Here is the press release: https://www.upmc.com/media/news/100615-invasive-lobular-breast-cancer
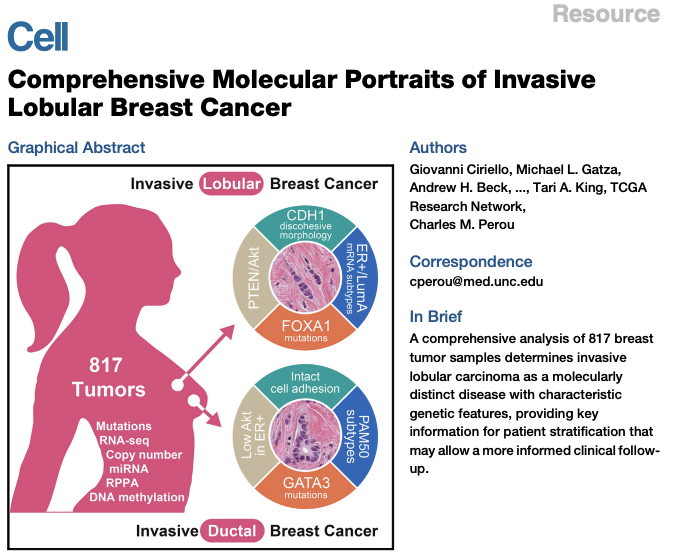
Dr. Oesterreich was honored and excited to join The Cancer Genome Atlas Network (TCGA) working group performing the largest to date comprehensive molecular analysis of ILC. This landmark paper provided a comprehensive molecular portrait of ILC, highlighting distinct genomic and transcriptomic features compared to invasive ductal carcinoma (IDC). Dr. Oesterreich contributed key expertise in lobular biology, ensuring that ILC was well represented within TCGA analyses, reflecting a major collaborative effort among over 50 institutions. The study showed that 95% of ILC cases had alterations in CDH1, that there were differences in mutations frequency (for example in PTEN, AKT, FOXA1 and TBX3), and that there are molecular variants within ILC. The conclusion was that “ILC is a clinically and molecularly distinct disease”.
An unbiased screen performed in Dr. Adrian Lee’s lab, identified E-cadherin as a top candidate interacting with the IGF1 pathway. Dr. Lee joined the ILC research efforts, which propelled ILC genomic studies in the now combined Lee-Oesterreich lab.
Dr. Oesterreich chaired the 1st International ILC Symposium held in Pittsburgh. We had approximately 130 attendees – physicians, researchers and patient advocates. This started a tradition of annual ILC Symposia, alternating in location between the US and Europe. This is where Dr. Oesterreich met Leigh Pate.
Dr. Steffi Oesterreich and Leigh Pate became good friends (and Leigh became a fierce yet humble ILC patient advocate). They had many phone calls and some in-person meetings discussing how to drive ILC research forward. Other patients who had joined the 1st ILC Symposium in 2016 in Pittsburgh joined in (such as Lori Pettiti) – and the Lobular Breast Cancer Alliance (LBCA) was born. Dr. Steffi Oesterreich served as Chair of the Scientific Advisory Board until 2022.
We had our first LBCA meeting, and LBCA poster at SABCS in 2017. Many patients with ILC became highly motivated and committed ILC advocates and spent countless hours working with Leigh Pate and Lori Petitti and others to get ILC advocacy off the ground.
Dr. Oesterreich gives a Keynote Lecture at the ILC Course in Boston in 2018, which starts the official continuation of the ILC Symposia. Drs. Otto Metzger and Rachel Jankowitz worked with some amazing advocates, including Julia Levine, Janice Axelroad, Lori Pettiti and Flora Migyanka (who later founded Dynami)
A breakout session at NWMBCC (hosted by Susan G. Komen Puget Sound) in which Dr. Steffi Oesterreich, Dr. Hannah Linden, and Leigh Pate discuss unique aspects of ILC (and a similar session). LBCA members discuss next steps for the organization, and Leigh Pate received the Beth Caldwell Advocacy and Leadership Award.
Limited availability of research models was a substantial barrier that at least partially accounted for the lack of research on ILC. Dr. Nilgun Tasdemir, a postdoc in the lab, performed a very elegant and thorough characterization of ILC cell lines – the start of our commitment to generate more ILC models faithfully representing different aspects of the disease. This project, with bioinformatics support from George Tseng, characterized 2D and 3D growth phenotypes of ILC cell lines. It emphasized how the unique morphology and cell–cell adhesion defects influence drug response and invasion, building a phenotypic framework for preclinical modeling.
San Antonio Breast Cancer Symposium 2018 has its first ILC-focused session, in which Dr. Oesterreich spoke about progress made understanding unique ILC biology.
We have had a number of productive collaborations with pharmaceutical companies, including Foundation Medicine. This study was the largest analysis of metastatic ILC at that point in time, and showed that mILC had an enrichment of NF1 mutations, and higher TMB (with APOBEC signature) compared to NST. Assessing sites of metastatic specimens showed fewer metastases in the liver and enrichment in reproductive sites, GI tract, omentum and bone marrow.
More LBCA meetings happened in which Dr. Steffi Oesterreich was happy to brainstorm with ILC patient advocates on best ways to get ILC to the forefront in research, clinical trials, meetings, education and more. Photo is taken at brainstorming session at Cleveland Clinic, organized by ILC Advocate Susan McDonald. Some of the ideas laid the foundation for the subsequent publication entitled Important “How Researchers, Clinicians and Patient Advocates Can Accelerate Lobular Breast Cancer Research” by Leigh Pate et al.
Using natural language processing, we screened more than 2 million de-identified patients records at UPMC in order to identify rare metastases to the eye. We identified 28 patients with orbital metastases, with a significant enrichment in patients with ILC. There was a trend that these metastases were more frequently bilateral, but less frequently co-occurring with metastases to the brain in ILC compared to NST, suggesting different routes of spread but larger studies combining data from multiple centers are necessary to confirm these findings.
Dr. Steffi Oesterreich and Dr. Adrian Lee receive funding from the NCI Oncology Models Forum to increase quality and quantity of ILC models: “Credentialing Models of Invasive Lobular Breast Cancer for Translational Research”– lack thereof was a critical hurdle for progress in ILC research.
Leigh Pate and Dr. Steffi Oesterreich had become close friends, and communicated often on how to partner researchers, clinicians and patient advocates. Together with other researchers and patient advocates they wrote a commentary putting forward a clear roadmap on how to make use of the unprecedented opportunity to drive forward multidisciplinary, multicenter and international collaborative research into ILC.
Due to Covid restrictions, we held the 2021 ILC Symposium (originally planned for Pittsburgh) virtually. Dr. Steffi Oesterreich worked with Drs. Otto Metzger, Christine Desmedt, and Patrick Derksen on the organization of the symposium which was a great success with more than 700 attendees from 36 countries.
Leigh Pate passes, which is not only an unsurmountable loss for the ILC patient advocacy community, but for ILC research. Her contributions to lobular breast cancer have affected the lives of thousands of patients and their families, and this number will only continue to grow. She left a donation to BCRF which started a project aimed at generation of ILC patient-derived organoids (PDOs). This is a collaboration between UPMC Hillman Cancer Center, Memorial Sloan Kettering Cancer Center and the Institute for Precision Medicine, which Dr. Adrian Lee directs. Dr. Lee has made the generation of patient-derived breast cancer organoids, spearheaded by Dr. Daniel Brown, a priority of IPM. Dr. Jagmohan Hooda in the Lee/Oesterreich lab leads the characterization of ILC PDOs and the collaboration effort with MSKCC.
Dr. Oesterreich is member of the ILCS Organizing Committee, along with Drs. Derksen, Desmedt, Salomon, Metzger, and Koorman, and as such helps to organize the 2022 ILCS in Utrecht, Netherlands.
In older women (≥70) with early-stage ER+ invasive lobular carcinoma (ILC), omitting sentinel lymph node biopsy (SLNB) was not associated with increased recurrence or worse locoregional recurrence-free survival compared to those who underwent SLNB, even though ILC patients presented with larger, higher-stage tumors. These findings support extending the Choosing Wisely recommendation to omit SLNB to patients with ILC, though larger studies and ongoing trials (SOUND, INSEMA) are needed to validate this conclusion.
A collaborative study between three founding members of the Great Lakes Breast Cancer Consortium – UPMC, Cleveland Clinic, and The James – identified meaningful differences in clinicopathological features between ILC and IDC/NST, analyzing data from more than 30,000 breast cancer patients. For patients with ILC we noted more lymph node involvement, diagnoses at later stage, higher grade and larger size tumors (with an increase over time), more mastectomies, and worse outcome – despite fewer cases with high recurrence scores.
Dr George Tseng, Professor in Biostatistics a UPitt, is a critical component of the Pittsburgh ILC Program of Excellence. His studies for testing congruence of ILC models with ILC clinical samples are critical for ILC research. For example, CASCAM (Congruence Analysis and Selection of Cancer Models) https://pubmed.ncbi.nlm.nih.gov/38198519/, helps to identify cell lines most representative for ILC research. He subsequently obtained an R01 grant (MPI with Dr. Adrian Lee) on “Single-cell congruence evaluation and selection of cancer models towards precision medicine”.
In a collaboration with the NSABP, we studied many clinico-pathological features of a large series of mixed ductal lobular cancer, and concluded that mixed IDC/ILC were more similar to ILC than IDC/NST. It is important to note that the WHO definition of mixed IDC/ILC has recently changed – the proportion of the special subtype in mixed tumors has decreased from 50% to 10%. It will be challenging to apply conclusions from our study to mixed cases with different definitions. These changes not only reflect the complicated nature of the mixed IDC/ILC tumors, but also the ever-changing definition. It is likely that the use of AI will help to clarify different ILC subtypes, including the mixed IDC/ILC cases.
This truly multi-disciplinary study with experts in immunology, bioinformatics, pathology and ILC allowed us to show that there were differences in immune infiltration between ER+ ILC and ER+ NST. While majority of ILC were “cold”, some were infiltrated with immune cells, dominated by M2-like macrophages. Spatial analyses identified neighborhoods with different prognosis in ILC vs NST.
Dr. Rohit Bhargava and his team identified a distinct breast cancer type called “lobular-like invasive mammary carcinomas” (LLIMCas) that resembles lobular cancers histologically but lacks their characteristic CDH1 gene mutations, instead showing CDH1 promoter methylation. LLIMCas are often underestimated on imaging with frequent positive margins, and thus Dr. Bhargava recommends recognizing them as a separate entity and using preoperative MRI to guide surgical management.
Dr. Oesterreich, several members of the Lee-Oesterreich Lab, and future ILC Program of Excellence team member Dr. Priscilla McAuliffe join the 2023 ILC Symposium Organizing Committee, helping organize and run the 2023 ILCS, which returns to Pittsburgh, PA.”
Together with Dr. Julia Foldi, Dr. Marija Balic is joining Dr. Adrian Lee’s longstanding efforts on the analysis of cfDNA in mILC, in part through the Apollo program
Together with patient advocates and leading ILC experts, we designed a survey in which with more than 1,700 (researchers, clinicians and patients) from 66 countries participated. Patients identified improvement of ILC screening/early detection, and development of better imaging tools as top research priorities. In contrast, both researchers and clinicians identified understanding of endocrine resistance and identifying novel drugs that can be tested in clinical trials as top research priority. Other research priorities included i) Dormancy, ii) ILC modeling, and ii) genomic predictors. Other noteworthy findings were that the majority of patients and advocates thought that their health care providers did not sufficiently explain the unique features of ILC, and that 85% of clinicians have never powered a clinical trial to allow subset analysis for histological subtypes, but the majority would consider it, and would participate in an ILC clinical trials consortium.
It remains challenging to understand and categorize mixed ductal lobular tumors. In this study, we utilized spatially resolved transcriptomic, genomic, and single-cell profiling for a comprehensive characterization of three mixed cases (categorized as such by three expert breast cancer pathologists at UPMC, UM and MSKCC). We identified clinically significant differences between ductal and lobular tumor regions including distinct intrinsic subtype heterogeneity – a finding that indicates challenges for prognosis and therapeutic decisions for these cases.
Dr. Oesterreich is again a member of the ILCS Organizing Committee, and as such helps to organize the 2024 ILCS in Leuven, Belgium.
Dr. Steffi Oesterreich and Dr. Adrian Lee are proud to mentor Dr. Julia Foldi, who arrived at UPMC in 2023 after finishing her breast medical oncology training at Yale. Dr. Foldi starts to focus her work on ILC, and in 2025 she opens a Liquid Biopsy trial for patients with metastatic ILC.
In this study, we performed a combined analysis of four NSABP trials with more than 12,000 patients treated with anthracycline-based adjuvant chemotherapy, and with at least 10 years of follow-up. While there was no significant difference in disease free survival and overall survival over the entire follow-up period, stratification by years since diagnosis showed that patients with ILC exhibited increased risk for late DFS events, recurrences, and deaths. We are currently expanding our correlative studies using the primary tumor specimens from this unique, large, annotated cohort of patients with ILC and matched NST with long-term follow up.
In a collaboration with Natera, we analyzed ctDNA longitudinally in 66 patients with metastatic ILC using tumor-informed Signatera assays. Sequencing results from N=355 samples showed that ctDNA testing is a promising approach for surveillance and precision medicine in patients with metastatic ILC, a setting where imaging has often limited sensitivity.
We held our first Celebration of Life event for families of patients enrolled in the Hope for OTHERS program, a rapid autopsy initiative designed to advance our understanding of treatment resistance and metastatic disease (described in https://pubmed.ncbi.nlm.nih.gov/40537829/). The success of the Hope for OTHERS program depends on key team members including Lori Miller, our clinical coordinator; Alex Chang, an MSTP student serving as our research coordinator; and dedicated patient advocates Christine Desmedt, Stephanie Walker, and Lori Livingston. Through the Hope for OTHERS program, we are collaborating with the UPTIDER program at KU Leuven, led by Dr. Christine Desmedt, to improve our understanding of metastatic ILC. A first combined manuscript is under review (Zels et al: Clinical and histopathological characterization of metastatic lobular breast cancer: lessons learned from post-mortem tissue donation programs).
The Pittsburgh ILC Program of Excellence was officially launched on October 15th, 2025, Global Lobular Breast Cancer Awareness Day. Pittsburgh’s ILC researchers, physicians, and patient advocates have formalized their long-standing collaboration into an official program dedicated to improving patient outcomes. This website documents our progress and keeps the research and patient community informed. The launch was planned and executed by a team consisting of Dr. Steffi Oesterreich, Dr. Adrian Lee, Dr. Jagmohan Hooda, Dr. Daniel Brown, Dr. Insa Thale, Hunter Waltermire, and Christopher Merkel.
On behalf of a large collaborative group of TBCRC investigators, as well as additional scientists working on the correlative studies, Dr. Oesterreich presented the ILC window trial (TBCRC037) at ESMO in Berlin. And we were happy that it won a BEST POSTER prize!
The ILC Think Tank, attended by 46 participants including 12 BCRF-funded investigators and held adjacent to the NYC BCRF meeting in October 2025, was considered highly successful, with its discussion-focused format fostering transparent and constructive dialogue on a number of critical topics including potential clinical trial targets and pathways. Three key proposals emerged from the meeting: forming a US-based ILC research working group, establishing an international ILC Association to strengthen collaboration with pharmaceutical partners, and identifying one or two urgent but achievable unmet needs that all attendees, or smaller subgroups, could address as a collaborative initiative.
Drs. Oesterreich and Kok (NKI) moderated an ILC session with exciting presentations by Drs. Vincent-Salomon, Metzger, Sotiriou, and Aftimos, as well as critical contributions from patient advocate Flora Migyanka. More details here: https://www.sabcsmeetingnews.org/special-session-amplifies-dialogue-on-lobular-breast-cancer/
Also, our team was proud to receive four LBCA Research Abstract Merit Awards for our ILC Posters presented at 2025 SABCS (Abdalla Wedn, Hannah Maynard, and Drs. Julia Foldi and Steffi Oesterreich).